IMPORTANT: Please Read This First
Caution: The relative ranking of myelofibrosis risk based on the following DIPSS scales — high, internediate, low — is considered accurate but survival estimates are highly variable based on individual genetics, clinical condition and the impact of new treatment protocols. Sharing results and questions with your hematologist is essential to develop a full picture of your status, prognosis, and treatment options
![]()
MAGIC, the MPN Assessment Graphic Internet Calculator, is a convenient and graphic means to summarize broad clinical experience in assessing overall risk-associated score for myelofibrosis, polycythemia vera and essential thrombocythemia.
MAGIC is an interactive MPN risk assessment tool, The actual determination of MPN risk of progression or assessment of the lethality of an MPN state is determined by multiple means such as blood tests, physical examination, bone marrow biopsy, genomic testing, pathology reports, etc.
What MAGIC offers is an overview of some major peeer-reviewed tests constructed and validated by MPN specialists. These test results have been found to statistically associate with MPN disease status. Taken into consideration with other clinical and genetic results – as well as patient reported symptoms – these tests help form the basis for diagnosis, anticipated prognosis and a treatment plan
Much about myeloproliferative neoplasm remains mysterious. Individual variations in response to the onset of disease and to treatment are great.
What MAGIC can provide is a snapshot of a patient’s current status based on available testing data.
For Myelofibrosis
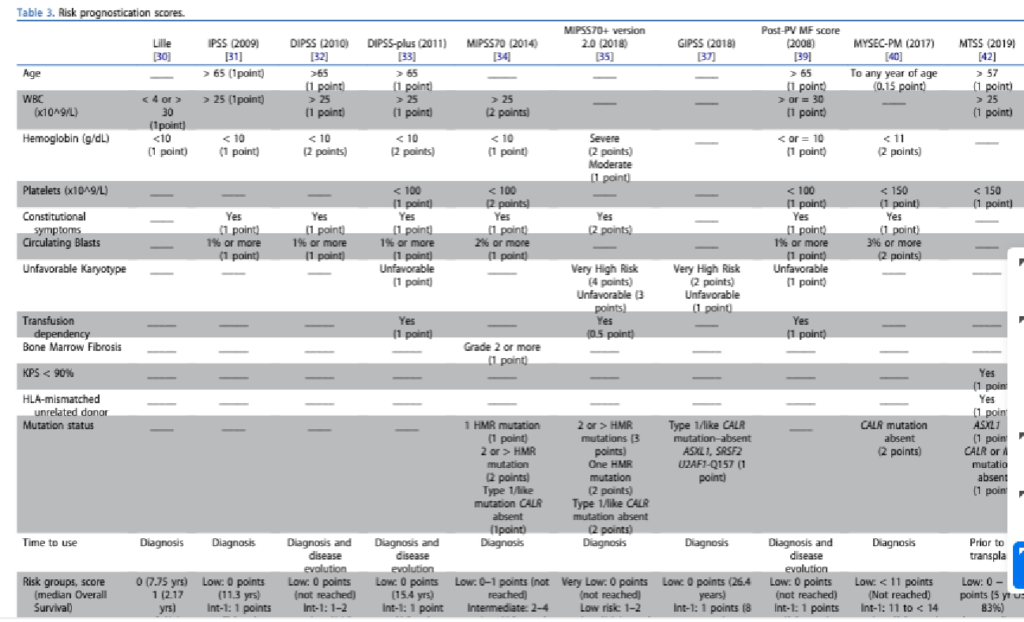
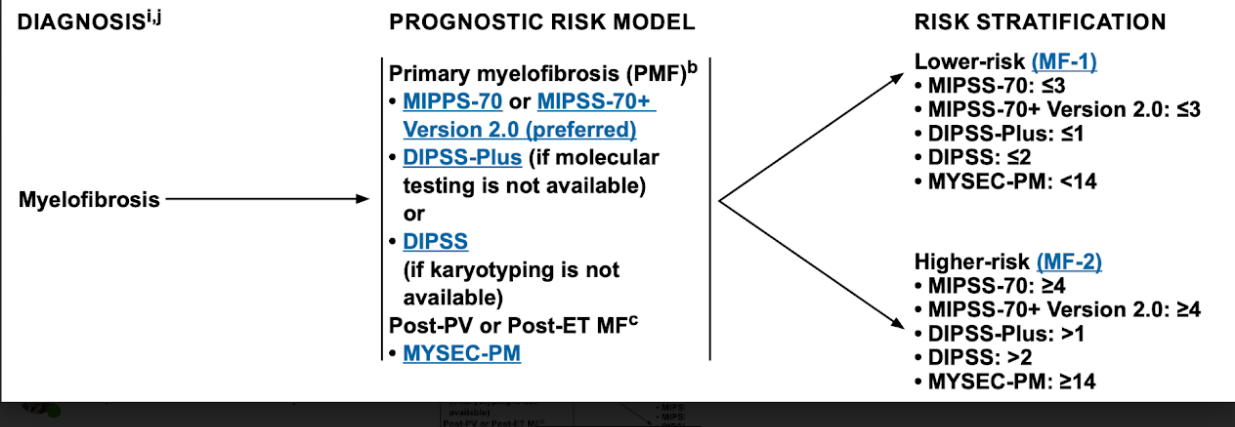
MAGIC relies on two commonly used and validated scales developed by the International Working Group on Myeloproliferative Neoplasms Research and Treatment (IWG-MRT). Together, the DIPSS (Dynamic International Prognostic Scoring System) and the DIPSS + assess the degree of myelofibrosis risk.*
There are four MF Risk Levels (Low, Intermediate-1, Intermed-2, and High) Each Risk Level carries a mean approximation of overall survival (OS) expressed in years and months. The OS is only a guideline. Mean survival is the midpoint between the number of those who will live longer and those who will die earlier.”
Myelofibrosis is a complex disease whose etiology and progression is only partially understood. Beyond the clinical elements measured by our scales, some factors influencing survival include genetics, environment, co-morbidities, diet, lifestyle, epigenetics, geography, occupation, and, emotional, social and psychological elements.
The MAGIC results are significant , however, in revealing a patient’s underlying general risk score and can serve as a guide to undertake minimal or more aggressive therapies.
For Polycythemia Vera, Essential Thrombocythemia and MF.
MAGIC includes reference to two clinically validated patient reported symptom scales, the MF-SAF and the MPN-SAF TSS, the myelofibrosis symptom assessemenz form and the MPN symptom assessment form — Total System Score.
The myelofibrosis symptom assessment form (Mesa et al., 2009, Leukemia Research) is “an evidence-based brief inventory to measure quality of life and symptomatic response to treatment in myelofibrosis.”
A brief history of the symptom burden assessment tools, along with sample forms, test scoring procedures and links to updates can be found here:
Expert Review of Hematology
Volume 13, 2020 – Issue 1
Review
Myelofibrosis: best practices, controversies and 2019
The Mutational Component
MAGIC provides the option for patients to select their known current MPN mutations. Calculation of the relative weight of these mutational selections has not been clinically validated. MAGIC currently relies only on the clinically validated DIPSS scales and the MPN-SAF to determine Risk Levels and Overall Survival averages for myelofibrosis and the MPN-SAF TSS scale for PV and ET.
The mutational landscape however provides vital prognostic information that may be applicable to selection of therapeutic options. In addition to the Notes on Individual Mutations included in the MAGIC text, links to new on-line calculators that do incorporate clinical, cytogenetic and mutational data are provided. Two of the most promising instruments that have already published results of extensive testing are the MIPSS70 and MIPSS70+ (P. Guglielmelli et al., Journal of Clinical Oncology, 2017.) and the MPN Personalized Risk Calculator (J. Grinfeld et al. New England Journal of Medicine, 2018).
Much has been learned about the role mutations play in the creation and driving of myeloproliferative neoplasms. Two recent studies – Vainchenker, Kralovics et al. and Grinfeld, Nangalia, et al. – were a primary basis for selecting commonly occurring driving and passenger mutations. And while there are both deadly and relatively benign mutations there remains some question as to the specific impact of any individual mutation. However, the presence of multiple mutations arising in an unstable genetic environment that includes MPN driving mutations generally predicts poor outcomes.
Three known MPN driving mutations – JAK2, CALR and MPL – are indicated in the tool’s graphic display with large, red markers. All other mutations are given equal weight although some are known to participate more often in progression to AML and others are more benign. Details and a full listing of all these mutations notes can be found in Notes on MPN Mutations an integral resource for MAGIC .